Epigastric pain is a common medical complaint that can be caused by a variety of underlying conditions. Understanding the causes, symptoms, and treatment options for epigastric pain is essential for both individuals experiencing this discomfort and healthcare professionals aiming to provide the best care. In this comprehensive article, we will delve into the details of epigastric pain, exploring its root causes, the telltale signs and symptoms, and the most effective treatment strategies. Let’s begin this journey to uncover the mysteries of epigastric pain.
Table of Contents
Introduction
Epigastric pain is a term frequently used in the medical field to describe discomfort or pain in the upper abdomen. It is important to understand the location of the epigastrium, which is the central, upper part of the abdomen, just below the ribcage. This area is home to several vital organs, making it a common site for various medical conditions to manifest as pain or discomfort.
Definition and Location
Epigastric pain is characterized by a burning, gnawing, or aching sensation in the epigastric region. The discomfort can vary in intensity, ranging from mild to severe, and may come and go or persist continuously. It is often described as a discomforting feeling that is usually located in the upper abdomen, right beneath the sternum (breastbone). The epigastrium is a critical anatomical region because it houses the:
- Stomach
- Part of the esophagus
- Part of the liver
- Gallbladder
- Pancreas
Understanding the location of the epigastrium is vital in recognizing the potential causes of epigastric pain, as discomfort in this area can be indicative of issues in any of the mentioned organs.
Importance of Understanding Epigastric Pain
Comprehending epigastric pain is crucial for both individuals and healthcare professionals. For individuals, it helps in recognizing when they need medical attention and seeking the right care promptly. For healthcare professionals, a deep understanding of epigastric pain is essential for accurate diagnosis and effective treatment. In the following sections, we will explore the common and less common causes of epigastric pain.
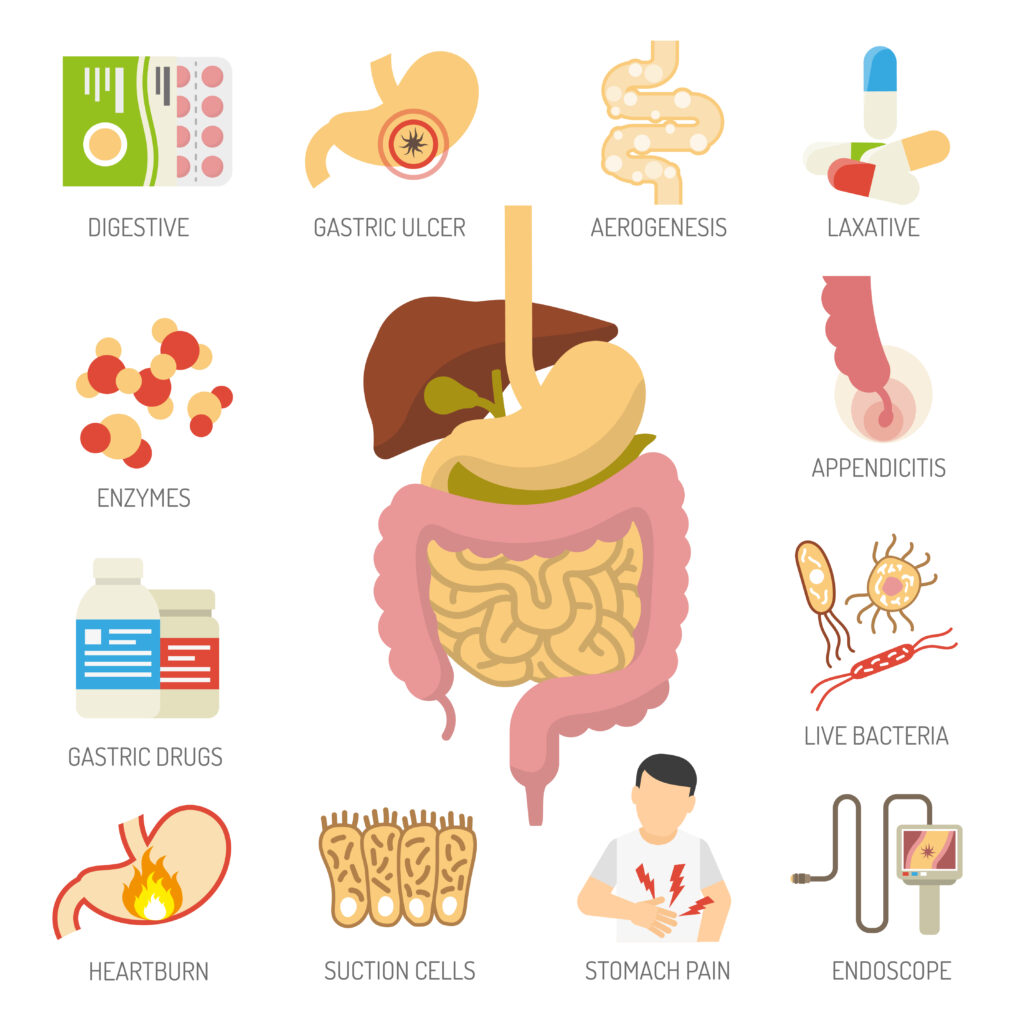
Common Causes of Epigastric Pain
Epigastric pain can result from various underlying medical conditions. Here, we will focus on the most common causes that individuals may encounter.
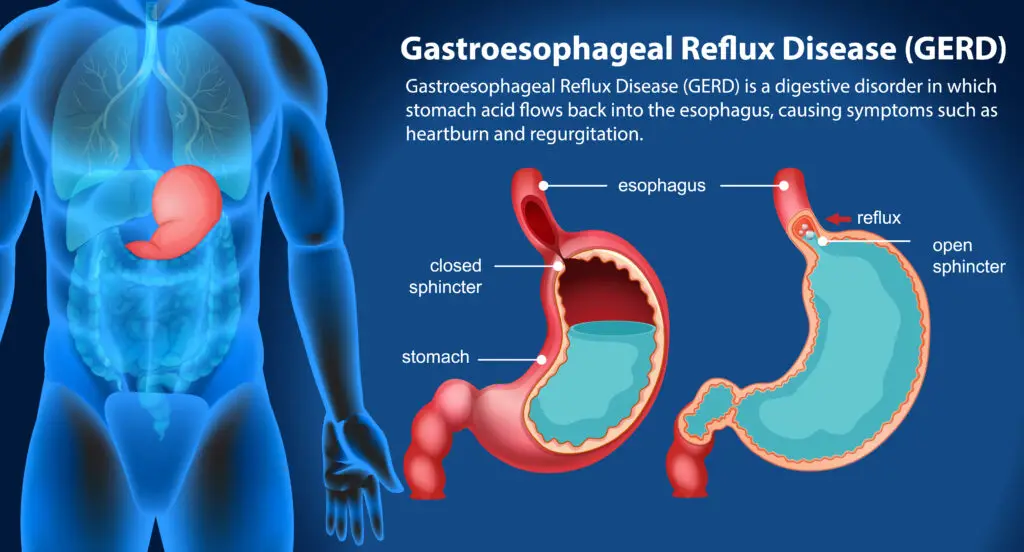
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease, commonly known as GERD, is a prevalent cause of epigastric pain. It occurs when stomach acid frequently flows back into the esophagus, causing irritation and inflammation. The epigastric pain associated with GERD is often described as a burning sensation that can radiate upwards towards the chest.
Peptic Ulcers
Peptic ulcers are sores that form on the lining of the stomach, small intestine, or esophagus. The pain from peptic ulcers typically presents as a gnawing or burning discomfort in the upper abdomen. These ulcers can be caused by bacterial infections or the use of nonsteroidal anti-inflammatory drugs (NSAIDs).
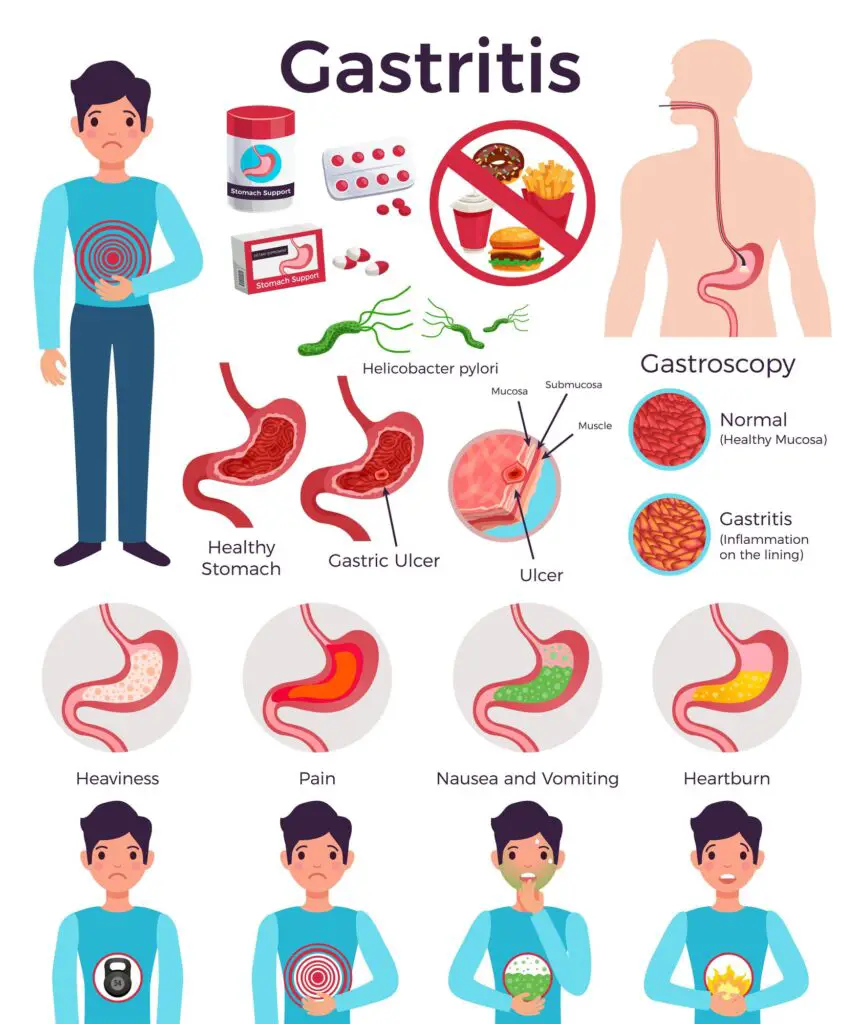
Gastritis
Gastritis occurs when the inner lining of your stomach gets inflamed. It can lead to epigastric pain, which is often characterized by a dull or burning sensation. Gastritis can be acute or chronic and is caused by various factors, including excessive alcohol consumption and certain medications.
Gallstones
Gallstones are hard particles that develop in the gallbladder. When a gallstone gets stuck in the bile duct, it can cause intense epigastric pain, known as biliary colic. The pain is typically sharp and can last for several hours.
Pancreatitis
Pancreatitis is when the pancreas, an organ situated behind your stomach, becomes inflamed. Epigastric pain from pancreatitis is severe and often described as a piercing, deep pain. Acute pancreatitis is a medical emergency that requires immediate attention.
Myocardial Ischemia
Myocardial ischemia occurs when the blood flow to the heart muscle is reduced. It can cause angina, which is characterized by chest pain or discomfort that can radiate to the epigastric region. This condition needs urgent medical evaluation.
Hiatal Hernia
A hiatal hernia happens when a portion of the stomach pushes up into the diaphragm through the hiatus. It can cause epigastric pain and may also result in acid reflux symptoms.
Less Common Causes of Epigastric Pain
In addition to the common causes mentioned above, there are less common conditions that can lead to epigastric pain. Understanding these less frequent culprits is essential for accurate diagnosis and treatment.
Esophagitis
Esophagitis is the inflammation of the esophagus. It can cause epigastric pain, often described as a burning sensation or discomfort behind the breastbone. This is often linked to a condition called gastroesophageal reflux disease (GERD).
Abdominal Aortic Aneurysm
An abdominal aortic aneurysm is a bulging or swelling of the aorta, the main blood vessel that supplies blood to the body. When this aneurysm ruptures, it can lead to severe, sudden epigastric pain and is a life-threatening emergency.
Pericarditis
Pericarditis is when the pericardium, which is the thin sac surrounding your heart, becomes inflamed. It can cause chest pain that radiates to the epigastric region. While pericarditis is rare, it requires medical evaluation.
Gastrointestinal Obstruction
A gastrointestinal obstruction happens when something is blocking the normal flow in your digestive system. It can lead to epigastric pain, often accompanied by vomiting and bloating. This condition is typically due to structural issues or adhesions.
Medication-Induced Epigastric Pain
Certain medications, particularly those that irritate the stomach lining, can cause epigastric pain. Nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and some antibiotics are known culprits.
Stress-Induced Epigastric Pain
Stress can manifest physically, and epigastric pain is one of the symptoms associated with stress. It is often described as a dull, aching discomfort in the upper abdomen.
Understanding the less common causes of epigastric pain is essential because it enables healthcare professionals to consider a broader range of possibilities when diagnosing patients. In the following sections, we will explore the symptoms of epigastric pain and when to seek medical attention.
Symptoms of Epigastric Pain
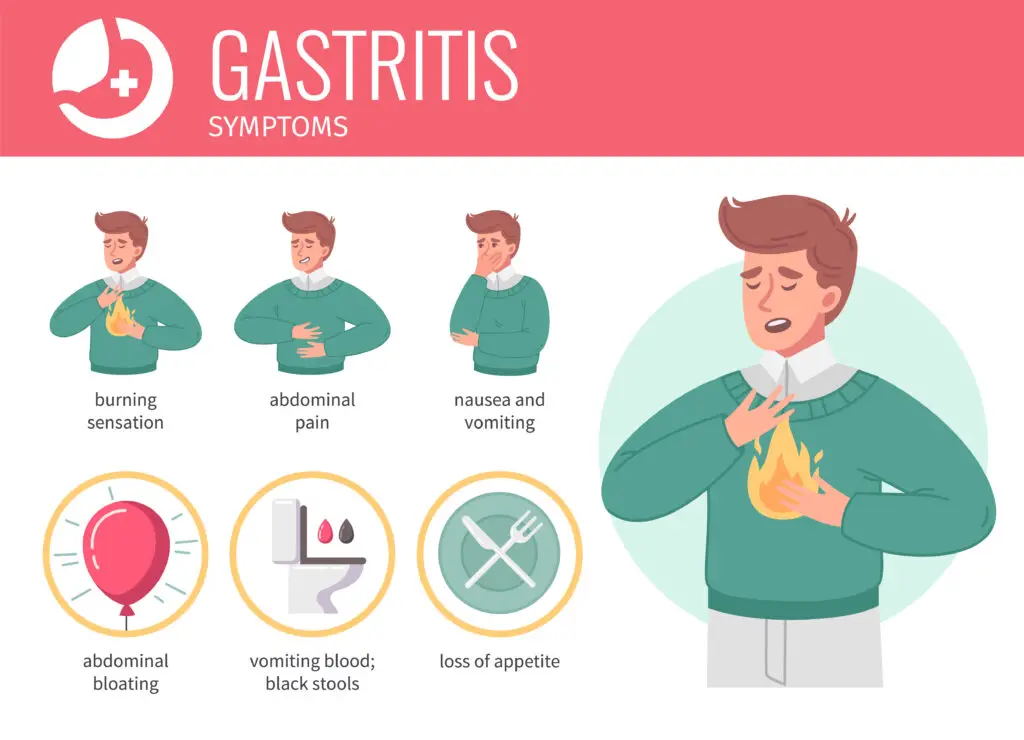
Recognizing the symptoms of epigastric pain is crucial in determining the underlying cause and seeking appropriate medical attention. Epigastric pain can manifest in various ways, and individuals may experience a combination of the following symptoms:
Burning Sensation
A burning sensation in the upper abdomen is one of the hallmark symptoms of epigastric pain. This discomfort is often described as a fiery or scalding feeling and can be a result of conditions like GERD, gastritis, or peptic ulcers.
Nausea and Vomiting
Epigastric pain may be accompanied by nausea and, in some cases, vomiting. The sensation of nausea can be quite distressing and is frequently seen in conditions like gallstone attacks or pancreatitis.
Bloating and Fullness
A feeling of bloating and fullness in the upper abdomen is another common symptom of epigastric pain. It can be associated with conditions such as gastritis or gastrointestinal obstruction.
Regurgitation
Regurgitation is the involuntary return of stomach contents into the esophagus or mouth. This can be a symptom of GERD, where stomach acid flows back into the esophagus, leading to a sour or bitter taste in the mouth.
Chest Discomfort
Epigastric pain may sometimes extend upwards and cause chest discomfort. This can be particularly alarming as it may mimic heart-related chest pain (angina). Understanding the differences between cardiac chest pain and epigastric pain is critical.
Belching
Excessive belching or burping can be a symptom of epigastric pain, especially in conditions like gastritis or hiatal hernia.
The combination of these symptoms can vary depending on the underlying cause of epigastric pain. It’s essential to pay attention to these signs and consult a healthcare professional when they persist or worsen.
When to Seek Medical Attention
While mild, occasional epigastric pain may not necessarily warrant immediate medical attention, certain factors should prompt individuals to seek help. It’s crucial to be aware of these red flags and indicators for when medical evaluation is necessary:
Alarm Symptoms
Certain symptoms should be considered alarm signals, indicating a need for urgent medical attention. These alarm symptoms include:
- Severe, unrelenting pain: If the epigastric pain is excruciating and unrelenting, it may indicate a severe underlying condition like a perforated ulcer or myocardial infarction.
- Difficulty swallowing: If the pain is associated with difficulty swallowing, it could be due to an obstruction or severe inflammation in the esophagus.
- Vomiting blood or black, tarry stools: This can be a sign of bleeding in the upper gastrointestinal tract, such as from an ulcer.
- Chest pain or pressure: If epigastric pain is accompanied by chest pain, especially if it radiates to the left arm or jaw, it can indicate a heart-related issue and requires immediate medical attention.
Duration and Frequency of Pain
The duration and frequency of epigastric pain are essential factors to consider. If the pain is persistent, severe, or recurrent, it should not be ignored. Frequent episodes of epigastric pain could signal a chronic condition that needs evaluation and treatment.
Impact on Daily Life
When epigastric pain interferes with daily activities, such as eating, sleeping, or working, it’s important to seek medical help. Persistent pain that affects one’s quality of life should not be dismissed.
In the next section, we will explore the diagnostic methods used to identify the underlying cause of epigastric pain.
Diagnosing Epigastric Pain
Diagnosing the cause of epigastric pain often involves a combination of medical history, physical examination, and various diagnostic tests. Healthcare professionals use these tools to pinpoint the underlying condition and determine the most appropriate treatment. Let’s delve into the diagnostic process.
Medical History and Physical Examination
Medical History
Gathering a detailed medical history is the first step in diagnosing epigastric pain. The healthcare provider will ask questions about the nature of the pain, its duration, any associated symptoms, and relevant medical history, such as a history of gastrointestinal issues, dietary habits, and medication use.
Physical Examination
A physical examination may reveal important clues about the cause of epigastric pain. The healthcare provider will examine the abdomen for tenderness, masses, or other abnormalities. They may also check for signs of dehydration, which can occur with vomiting.
Imaging Studies
Imaging studies are often used to visualize the structures within the abdomen and identify any abnormalities that may be causing epigastric pain. Common imaging tests include:
1. X-ray: An abdominal X-ray can help detect issues such as bowel obstructions, gallstones, or foreign objects.
2. Ultrasound: Abdominal ultrasound is a non-invasive imaging technique that can reveal gallstones, liver or pancreas abnormalities, and more.
3. Endoscopy: During an upper endoscopy, a thin, flexible tube with a camera is inserted through the mouth to examine the esophagus, stomach, and upper small intestine. This can help identify conditions like esophagitis, gastritis, and peptic ulcers.
4. CT Scan: A computed tomography (CT) scan provides detailed cross-sectional images of the abdominal organs, helping in the diagnosis of conditions such as pancreatitis, abdominal aortic aneurysm, and gastrointestinal obstructions.
Laboratory Tests
Laboratory tests can provide valuable information about the cause of epigastric pain. Common tests include:
1. Blood Tests: Blood tests can reveal elevated levels of specific enzymes or markers associated with conditions like pancreatitis or myocardial infarction.
2. Stool Tests: Stool tests can detect blood in the stool, which may suggest gastrointestinal bleeding.
3. H. pylori Testing: Helicobacter pylori is a bacterium associated with the development of peptic ulcers. Testing for H. pylori infection may be recommended in cases of chronic epigastric pain.
Once a diagnosis is made, healthcare providers can develop a treatment plan tailored to the specific underlying cause of epigastric pain. In the following sections, we will explore the various treatment options available.

Treatment Options
The treatment of epigastric pain depends on the underlying cause. It’s important to note that effective management of epigastric pain often involves a combination of lifestyle changes, medications, and, in some cases, surgical interventions. Let’s explore the treatment options for different causes of epigastric pain.
Lifestyle Modifications
For many individuals with epigastric pain, especially those with conditions like GERD or gastritis, lifestyle modifications can make a significant difference in symptom management. These changes may include:
- Dietary Adjustments: Avoiding trigger foods that worsen symptoms, such as spicy, acidic, and fatty foods.
- Eating Smaller, Frequent Meals: This can help reduce the pressure on the stomach and alleviate discomfort.
- Weight Management: Maintaining a healthy weight can decrease pressure on the abdomen, which is beneficial for conditions like hiatal hernia.
- Elevating the Head of the Bed: This can help reduce nighttime symptoms of GERD by preventing stomach acid from flowing back into the esophagus.
Medications
Medications play a crucial role in managing epigastric pain and its underlying causes. The type of medication prescribed will depend on the specific condition. Common medications include:
- Antacids: Over-the-counter antacids can provide relief from heartburn and indigestion.
- Proton Pump Inhibitors (PPIs): These medications reduce stomach acid production and are often used to treat conditions like GERD and peptic ulcers.
- H2 Blockers: H2 blockers can help reduce stomach acid and alleviate symptoms of conditions like GERD and peptic ulcers.
- Antibiotics: Antibiotics may be prescribed to treat Helicobacter pylori infection in cases of peptic ulcers.
- Pain Relievers: For mild epigastric pain, over-the-counter pain relievers like acetaminophen may be recommended.
- Pancreatic Enzyme Replacement: In cases of chronic pancreatitis, enzyme replacement therapy may be necessary to aid digestion.
- Medications for Cardiac Conditions: If myocardial ischemia is the cause of epigastric pain, medications to manage heart conditions will be prescribed.
Surgery
In some cases, surgical intervention may be necessary to address the underlying cause of epigastric pain. Common scenarios in which surgery may be recommended include:
- Gallstones: Surgical removal of the gallbladder (cholecystectomy) is often necessary when gallstones are causing recurrent epigastric pain.
- Gastroesophageal Reflux Disease (GERD): For severe GERD that does not respond to medication or lifestyle changes, surgical procedures like fundoplication may be recommended to prevent acid reflux.
- Perforated Ulcer: Emergency surgery is essential if an ulcer perforates, causing severe abdominal pain and infection.
The decision to pursue surgical treatment is typically made in consultation with a healthcare provider and is based on the specific diagnosis and individual circumstances.
Alternative and Complementary Therapies
In addition to conventional medical treatments, some individuals explore alternative and complementary therapies to manage their epigastric pain. These therapies can include:
- Acupuncture: Acupuncture may provide relief for some individuals with epigastric pain, especially when related to stress or functional gastrointestinal disorders.
- Herbal Remedies: Certain herbal remedies, such as ginger or peppermint, are known for their potential to ease digestive discomfort.
- Meditation and Yoga: These relaxation techniques can help manage stress, which can exacerbate epigastric pain.
- Probiotics: Probiotic supplements or foods containing beneficial bacteria may help support digestive health.
It’s essential to consult with a healthcare provider before pursuing alternative therapies to ensure they are safe and appropriate for your specific condition.
In the next section, we will delve into how individuals can manage and prevent epigastric pain at home, with a focus on dietary changes, over-the-counter medications, and stress management techniques.
Managing Epigastric Pain at Home
Managing epigastric pain at home involves several strategies aimed at reducing discomfort and preventing the recurrence of symptoms. These strategies may vary depending on the underlying cause of the pain. Here are some general approaches:
Dietary Changes
For many individuals, dietary adjustments can significantly improve epigastric pain. Consider the following recommendations:
- Avoid Trigger Foods: Identify and avoid foods that trigger or worsen your symptoms. Common culprits include spicy foods, caffeine, alcohol, and acidic foods.
- Smaller, Frequent Meals: Instead of large, heavy meals, opt for smaller, more frequent meals to reduce the pressure on the stomach.
- High-Fiber Diet: Incorporate fiber-rich foods like fruits, vegetables, and whole grains to support digestion.
- Hydration: Drink plenty of water to stay hydrated, but avoid excessive consumption during meals, as it can lead to bloating.
- Dietary Restrictions: If you have a specific condition like celiac disease or lactose intolerance, adhere to dietary restrictions recommended by your healthcare provider.
Over-the-Counter Medications
For mild epigastric pain, over-the-counter (OTC) medications can provide relief. These may include:
- Antacids: Antacids can help neutralize stomach acid and alleviate heartburn and indigestion.
- H2 Blockers: Histamine-2 (H2) receptor antagonists, available without a prescription, can reduce stomach acid production.
- Pain Relievers: OTC pain relievers like acetaminophen can help manage mild discomfort.
Stress Management
Stress can exacerbate epigastric pain, especially in cases where no underlying physical cause is found. To manage stress and its impact on your digestive system, consider:
- Relaxation Techniques: Practicing relaxation techniques such as deep breathing, meditation, or progressive muscle relaxation.
- Yoga: Engaging in yoga sessions, which can promote relaxation and reduce stress.
- Counseling: If stress is a significant factor in your epigastric pain, consider seeking the support of a mental health professional for counseling.
These home management strategies can be particularly helpful for individuals with conditions like functional gastrointestinal disorders, where stress plays a prominent role in symptom exacerbation.
In the next section, we will explore strategies for preventing epigastric pain, including adopting healthy eating habits, managing weight, and reducing stress.

Preventing Epigastric Pain
Preventing epigastric pain involves adopting a proactive approach to your health and well-being. By implementing certain lifestyle changes and habits, you can reduce the risk of experiencing this discomfort. Here are some effective preventive strategies:
Healthy Eating Habits
Maintaining a healthy diet is key to preventing epigastric pain. Consider the following dietary guidelines:
- Balanced Diet: Consume a balanced diet rich in fruits, vegetables, lean proteins, and whole grains.
- Hydration: To keep yourself well-hydrated, make sure to drink a sufficient amount of water throughout the day.
- Fiber Intake: Incorporate high-fiber foods into your diet to support healthy digestion.
- Portion Control: Be mindful of portion sizes to prevent overeating, which can contribute to indigestion.
Weight Management
Maintaining a healthy weight is essential for preventing epigastric pain, particularly in cases related to hiatal hernia and GERD. Weight management strategies include:
- Regular Exercise: Engage in regular physical activity to help maintain a healthy weight and support overall health.
- Consult a Dietitian: If you struggle with weight management, consider consulting a dietitian for personalized guidance.
Stress Reduction
Stress can exacerbate epigastric pain, so it’s important to implement stress reduction techniques, such as:
- Stress Management Techniques: Learn and practice stress management techniques like deep breathing, mindfulness, and meditation.
- Exercise: Physical activity is an excellent way to reduce stress and promote emotional well-being.
- Counseling: Consider counseling or therapy if you have ongoing stress-related issues that impact your health.
By incorporating these preventive measures into your daily life, you can significantly reduce the likelihood of experiencing epigastric pain. However, it’s important to remember that some causes of epigastric pain, such as gallstones or peptic ulcers, may not be preventable through lifestyle changes alone. Seeking timely medical attention is crucial in such cases.
The Role of Stress in Epigastric Pain
Stress plays a significant role in the development and exacerbation of epigastric pain, particularly in cases where no clear physical cause is found. The gut-brain connection, often referred to as the “enteric nervous system,” is a complex network of nerves that links the brain and the gastrointestinal system.
The Gut-Brain Connection
The gut-brain connection involves bidirectional communication between the central nervous system (CNS) and the enteric nervous system (ENS), which is sometimes referred to as the “second brain.” This connection allows the brain to influence gastrointestinal function, and vice versa.
When you experience stress or anxiety, it can impact your gastrointestinal system in several ways, including:
- Altered Gut Motility: Stress can lead to changes in gut motility, potentially causing diarrhea or constipation.
- Increased Sensitivity: Stress can make the gastrointestinal tract more sensitive, which can lead to heightened awareness of sensations like epigastric pain.
- Inflammation: Chronic stress may contribute to inflammation in the gut, which can exacerbate conditions like gastritis or irritable bowel syndrome (IBS).
Coping Mechanisms
Given the significant impact of stress on the gastrointestinal system, it’s crucial to develop effective coping mechanisms. Some strategies for managing stress and its impact on epigastric pain include:
- Mindfulness Meditation: Mindfulness meditation means focusing on the here and now without passing judgment. It’s a way to lower stress and encourage relaxation.
- Yoga: Yoga combines physical postures, breathing exercises, and meditation to reduce stress and improve overall well-being.
- Deep Breathing: Deep breathing exercises can be practiced anywhere and are effective in reducing stress.
- Counseling: If stress is a persistent issue, consider seeking the support of a mental health professional for counseling or therapy.
Understanding the role of stress in epigastric pain is essential for individuals looking to manage their symptoms effectively. By incorporating stress reduction techniques into their daily routine, many individuals can experience significant relief.
Specific Treatment Approaches for Common Causes
Now, let’s explore specific treatment approaches for the most common causes of epigastric pain. Tailoring treatment to the underlying cause is vital for successful management.
GERD Treatment
Lifestyle Modifications
- Dietary Changes: Avoid trigger foods, eat smaller meals, and reduce alcohol and caffeine consumption.
- Weight Management: Maintain a healthy weight to reduce pressure on the stomach.
- Elevate the Head of the Bed: This can help prevent nighttime acid reflux.
Medications
- Antacids: Over-the-counter antacids can provide quick relief.
- Proton Pump Inhibitors (PPIs): PPIs are often prescribed to reduce stomach acid production.
- H2 Blockers: H2 blockers can also be effective in managing symptoms.
Surgery
- Fundoplication: In severe cases of GERD that do not respond to medications, fundoplication surgery may be considered to prevent acid reflux.
Peptic Ulcer Management
Medications
- Antibiotics: If the ulcer is caused by H. pylori infection, a combination of antibiotics may be prescribed to eradicate the bacteria.
- Proton Pump Inhibitors (PPIs): PPIs can help reduce stomach acid and promote ulcer healing.
- H2 Blockers: H2 blockers may be used in conjunction with PPIs.
Lifestyle Modifications
- Avoid NSAIDs: If NSAIDs are a contributing factor, avoid their use.
- Smoking Cessation: Quit smoking, as it can exacerbate peptic ulcers.
Surgery
- Surgery for Complications: In cases of complications like perforation or bleeding ulcers, emergency surgery may be required.
Gastritis and Its Remedies
Medications
- Acid Suppressors: Medications that reduce stomach acid production, such as PPIs or H2 blockers, can help alleviate gastritis symptoms.
Lifestyle Modifications
- Dietary Changes: Avoiding trigger foods and irritants.
- Stress Reduction: Implement stress management techniques to minimize stress-induced gastritis.
Gallstone Treatments
Surgery
- Cholecystectomy: Surgical removal of the gallbladder is the most common treatment for gallstones, especially when they cause recurrent pain.
Pancreatitis Interventions
Hospitalization
- Fluid and Nutritional Support: Hospitalization is often necessary to provide fluids and nutrition through intravenous (IV) methods.
- Pain Management: Pain control is a crucial aspect of pancreatitis treatment.
Managing Myocardial Ischemia
Cardiac Interventions
- Angioplasty: In cases of coronary artery blockages, angioplasty with stent placement may be performed.
- Medications: Medications to improve blood flow to the heart and reduce heart workload may be prescribed.
Hiatal Hernia Solutions
Lifestyle Modifications
- Dietary Changes: Avoid trigger foods and overeating.
- Weight Management: Maintain a healthy weight to reduce pressure on the hiatus.
Medications
- Antacids and H2 Blockers: These medications can help manage symptoms of acid reflux associated with hiatal hernias.
The specific treatment approach for each common cause of epigastric pain is tailored to the individual and the severity of their condition. Consultation with a healthcare provider is essential to determine the most appropriate course of action.
In the next section, we will explore medical interventions for less common causes of epigastric pain.
Medical Interventions for Less Common Causes
While less common, some causes of epigastric pain may require specific medical interventions. Let’s explore how healthcare professionals address these less frequent culprits of epigastric discomfort.
Addressing Esophagitis
Medications
- Proton Pump Inhibitors (PPIs): PPIs are commonly prescribed to reduce stomach acid and promote healing of the esophagus in cases of esophagitis.
- H2 Blockers: H2 blockers can also be used to reduce acid production and alleviate symptoms.
Lifestyle Modifications
- Dietary Changes: Avoiding acidic, spicy, or trigger foods to reduce irritation.
- Weight Management: Maintaining a healthy weight to minimize pressure on the stomach.
Treating Abdominal Aortic Aneurysms
Surgery
- Aneurysm Repair: The main treatment for abdominal aortic aneurysms is surgery to repair or replace the weakened or bulging section of the aorta.
Managing Pericarditis
Medications
- Anti-Inflammatory Drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to reduce inflammation and alleviate pericarditis symptoms.
Lifestyle Modifications
- Rest: Adequate rest and avoiding strenuous activities can help in the management of pericarditis.
Surgical Options for Gastrointestinal Obstruction
Surgery
- Removal of Obstruction: Surgical intervention is often required to remove the obstruction in cases of gastrointestinal blockages.
Medication Adjustments
When epigastric pain is induced or exacerbated by certain medications, healthcare professionals may consider adjusting or discontinuing the offending drugs and exploring alternative treatment options.
Stress Reduction Techniques
In cases of stress-induced epigastric pain, individuals are encouraged to explore stress reduction techniques, including mindfulness, meditation, and counseling.
Understanding the less common causes of epigastric pain and the associated medical interventions is crucial for both individuals and healthcare providers. It ensures that accurate diagnosis and effective treatment are pursued.
In the next section, we will explore the potential complications of untreated epigastric pain and why timely medical intervention is essential.
Complications of Untreated Epigastric Pain
Untreated or poorly managed epigastric pain can lead to a range of complications, some of which can be severe and life-threatening. Understanding these potential complications underscores the importance of seeking timely medical attention when experiencing epigastric pain.
Esophageal Damage
Untreated conditions like GERD or severe esophagitis can lead to damage of the esophagus. Over time, repeated exposure to stomach acid can cause erosions, ulcers, and strictures (narrowing of the esophagus), making swallowing difficult and painful.
Bleeding Ulcers
Peptic ulcers left untreated can bleed, leading to potentially life-threatening gastrointestinal bleeding. This can manifest as vomiting blood or having black, tarry stools, which are alarming signs that require immediate medical attention.
Perforation
In cases of severe peptic ulcers, a rupture or perforation can occur. This is a medical emergency and can lead to life-threatening infection and severe abdominal pain.
Pancreatic Complications
Chronic pancreatitis, if not managed appropriately, can lead to complications such as pancreatic pseudocysts or chronic pain, significantly impacting an individual’s quality of life.
Cardiac Events
For individuals with undiagnosed or untreated myocardial ischemia, there is an increased risk of experiencing heart attacks or other cardiac events. Timely medical intervention is critical in these cases to prevent severe consequences.
Understanding these potential complications serves as a stark reminder of the importance of promptly seeking medical attention when experiencing epigastric pain. In the next section, we will explore the significance of follow-up care.
The Importance of Follow-Up Care
Continued care plays a crucial role in handling epigastric pain, especially for persistent or recurring conditions. Healthcare providers schedule follow-up appointments to track your progress, make any necessary treatment adjustments, and prevent potential complications. Let’s explore why follow-up care is so important:
Monitoring Progress
Follow-up appointments allow healthcare providers to assess how well the treatment is working. Patients can report any changes in their symptoms, and providers can perform physical examinations to track improvements or identify any new issues.
Medication Adjustments
In cases where medication is part of the treatment plan, follow-up appointments provide an opportunity to review the effectiveness of the prescribed drugs. Providers may need to adjust the type or dosage of medications to optimize symptom management.
Preventing Recurrence
For conditions like GERD or peptic ulcers, follow-up care is important to prevent recurrence. By monitoring the patient’s condition, healthcare providers can identify any signs of relapse and take preventive measures.
Ensuring that patients attend follow-up appointments as recommended is vital for the long-term management of epigastric pain. In the next section, we will explore the circumstances in which surgery is necessary to address epigastric pain.
When Surgery is Necessary
Surgery for epigastric pain may be necessary in specific situations, depending on the underlying cause and the patient’s overall health. Here are some circumstances in which surgery may be recommended:
Indications for Surgery
Gallstones
- Recurrent Symptoms: If an individual experiences recurrent gallstone-related epigastric pain, surgery to remove the gallbladder (cholecystectomy) may be recommended to prevent future attacks.
Gastroesophageal Reflux Disease (GERD)
- Ineffectiveness of Medications: When medications and lifestyle changes do not adequately control GERD symptoms, surgical options like fundoplication may be considered.
Peptic Ulcers
- Perforation or Bleeding: In cases of ulcers that have perforated or are actively bleeding, emergency surgery is necessary to repair the damage.
Hiatal Hernia
- Severe Symptoms: Surgery may be considered for individuals with severe hiatal hernia symptoms that do not respond to conservative treatment.
Abdominal Aortic Aneurysm
- Aneurysm Repair: Aneurysms that are at risk of rupture require surgical repair.
Pancreatitis
- Complications: In cases of severe acute pancreatitis with complications like infected pancreatic necrosis, surgery may be needed to remove dead tissue.
Gastrointestinal Obstruction
- Blockage Removal: Surgical intervention is often the most effective way to remove obstructions in the digestive tract.
The decision to proceed with surgery is typically made in consultation with a healthcare provider, taking into account the patient’s overall health and the specific circumstances of their condition. In the final section, we will recap the key points regarding epigastric pain and the importance of early diagnosis and treatment.

Alternative and Complementary Therapies
In addition to conventional medical treatments, some individuals explore alternative and complementary therapies to manage their epigastric pain. These therapies can offer holistic approaches to address the discomfort and improve overall well-being. It’s important to note that while these approaches may provide relief for some individuals, they should be used in consultation with a healthcare provider and are not a replacement for medical treatment. Here are some alternative and complementary therapies that are commonly considered:
- Acupuncture: Acupuncture involves the insertion of thin needles into specific points on the body. Many believe it aids in balancing your energy and supporting the healing process. Some individuals find relief from epigastric pain, particularly when it is related to stress or functional gastrointestinal disorders, through acupuncture.
- Herbal Remedies: Herbal remedies have been used for centuries to alleviate various ailments. Ginger, for example, is known for its potential to ease digestive discomfort. Peppermint and chamomile teas are also popular choices for soothing the stomach. However, it’s essential to use herbal remedies cautiously, as they can interact with medications and may not be suitable for everyone.
- Meditation and Yoga: Stress management is a key aspect of reducing epigastric pain, especially when stress is a contributing factor. Meditation and yoga are relaxation techniques that can help manage stress, promote emotional well-being, and improve overall health. Engaging in regular meditation or yoga sessions can be beneficial for individuals dealing with stress-related epigastric discomfort.
- Probiotics: Probiotics are supplements or foods that contain beneficial bacteria, which can help support digestive health. Some individuals with gastrointestinal issues find relief from symptoms by incorporating probiotics into their daily routine. These supplements aim to maintain a healthy balance of gut bacteria, which can contribute to improved digestion.
It’s important to discuss the use of alternative and complementary therapies with a healthcare provider to ensure that they are safe and appropriate for your specific condition. In some cases, these therapies can complement traditional medical treatments, providing a well-rounded approach to managing epigastric pain.
Epigastric Pain in Pregnancy
Pregnancy is a unique period in a woman’s life, marked by significant physiological and hormonal changes. These changes can sometimes lead to epigastric pain, which is not uncommon during pregnancy. Understanding the causes and management of epigastric pain in pregnancy is essential for expectant mothers.
Causes of Epigastric Pain in Pregnancy
- Gastroesophageal Reflux Disease (GERD): Hormonal changes during pregnancy can relax the lower esophageal sphincter, allowing stomach acid to flow back into the esophagus, resulting in heartburn and epigastric discomfort.
- Increased Intra-abdominal Pressure: As the uterus expands to accommodate the growing baby, it can exert pressure on the stomach, leading to epigastric pain.
- Gallbladder Issues: Pregnancy hormones can lead to the formation of gallstones, which may cause gallbladder-related epigastric pain.
- Constipation: Hormonal changes and pressure on the intestines can slow down the digestive system, leading to constipation and abdominal discomfort.
- Preeclampsia: In some cases, epigastric pain may be a sign of preeclampsia, a pregnancy complication characterized by high blood pressure and damage to organs, such as the liver.
Managing Epigastric Pain During Pregnancy
- Dietary Modifications: Avoiding spicy and fatty foods, as well as large meals, can help reduce the likelihood of heartburn and indigestion. Eating smaller, more frequent meals may also alleviate stomach pressure.
- Elevating the Head of the Bed: Sleeping with the upper body elevated can help prevent acid reflux during the night.
- Antacids: Over-the-counter antacids may provide relief from heartburn, but it’s important to consult with a healthcare provider before using any medications during pregnancy.
- Drinking Water: Staying hydrated and consuming adequate amounts of water can help prevent constipation.
- Consulting a Healthcare Provider: If epigastric pain during pregnancy is severe, persistent, or accompanied by other concerning symptoms, it’s crucial to consult a healthcare provider. They can rule out any serious conditions and provide appropriate guidance and treatment.
Epigastric pain during pregnancy is generally a common and manageable discomfort. However, it’s essential to communicate any unusual or severe symptoms with a healthcare provider to ensure both the mother’s and baby’s well-being.
Epigastric Pain in Pregnancy: When to Seek Medical Attention
While epigastric pain during pregnancy is often benign and related to the physiological changes of gestation, there are instances where it may signal a more serious condition. Expectant mothers should be vigilant about their health and promptly seek medical attention if they experience the following symptoms:
- Severe or Prolonged Pain: If the epigastric pain is severe, persistent, or worsening, it could be a sign of a more serious issue that requires medical evaluation.
- Vomiting Blood or Dark Stools: These symptoms may indicate gastrointestinal bleeding, which should be addressed immediately.
- Swelling and High Blood Pressure: Sudden swelling, especially in the hands and face, accompanied by high blood pressure, may be indicative of preeclampsia, a potentially life-threatening condition.
- Jaundice: Yellowing of the skin or eyes could signal a liver problem, which requires medical assessment.
- Inability to Keep Food Down: If severe nausea and vomiting persist, it could lead to dehydration and may require medical intervention.
- Fever: The presence of a fever alongside epigastric pain may indicate an infection or other underlying issue.
- Decreased Fetal Movement: A noticeable reduction in fetal movement should be reported to a healthcare provider.
- Breathing Difficulties: If epigastric pain is associated with severe shortness of breath, it may be a sign of a more significant problem, such as pulmonary issues or heart-related concerns.
In all cases, pregnant individuals should have open communication with their healthcare providers and promptly report any unusual or concerning symptoms. Timely medical evaluation and intervention are crucial to ensure the health and well-being of both the expectant mother and the developing baby.
Support and Coping Strategies
Dealing with epigastric pain, whether it is an acute episode or a chronic condition, can be challenging. However, there are various support and coping strategies that can help individuals manage their discomfort and improve their quality of life. Here are some effective ways to cope with epigastric pain:
1. Seek Medical Guidance: The first and most crucial step in coping with epigastric pain is to seek medical advice. A healthcare provider can accurately diagnose the underlying cause and recommend appropriate treatments. Maintaining open and honest communication with your healthcare providers is crucial.
2. Medication Management: If prescribed medications are part of your treatment plan, ensure that you take them as directed. It’s important not to skip doses or discontinue medication without consulting your healthcare provider.
3. Lifestyle Modifications: Implementing lifestyle changes can make a significant difference. This may include dietary adjustments, stress management techniques, and maintaining a healthy weight. Your healthcare provider can offer guidance on the specific changes you should make.
4. Stress Reduction: Stress is a common exacerbating factor for epigastric pain. Engaging in stress reduction techniques such as mindfulness meditation, yoga, and deep breathing exercises can help manage stress and alleviate symptoms.
5. Dietary Awareness: Be mindful of your diet and identify trigger foods that may worsen your symptoms. Common triggers include spicy, fatty, and acidic foods. Reducing your intake of these items can lead to symptom improvement.
6. Support Groups: Joining a support group or community of individuals who share similar health concerns can be immensely beneficial. It provides a platform to exchange experiences, seek advice, and find emotional support from those who understand what you’re going through.
7. Mind-Body Practices: Practices like meditation, guided imagery, and relaxation exercises can help alleviate pain and reduce stress. These techniques promote a sense of calm and well-being.
8. Regular Exercise: Engaging in regular physical activity can improve overall health and well-being. However, consult your healthcare provider before starting any new exercise routine, as intense physical activity may exacerbate certain conditions.
9. Educate Yourself: Understanding the underlying cause of your epigastric pain and the treatment options available can empower you to take an active role in your healthcare. Stay informed and ask questions during medical appointments.
10. Medication Record: Maintain a record of your medications, including the names, dosages, and schedules. This can help you stay organized and ensure you take your medications as prescribed.
11. Keep a Symptom Journal: A symptom journal can help you track your epigastric pain and identify patterns or triggers. It can also serve as a valuable resource during medical appointments, enabling you to provide detailed information about your symptoms.
12. Ask for Help: Don’t hesitate to ask for support from friends and family. They can provide emotional support, assist with daily tasks during painful episodes, and be there to listen when you need to talk.
13. Pain Management Techniques: If your pain is severe, consider exploring pain management techniques such as heat therapy or cold packs. These methods can provide temporary relief.
14. Consult a Mental Health Professional: Chronic pain can take a toll on your mental well-being. If you find yourself struggling with anxiety, depression, or other emotional challenges, consider consulting a mental health professional for guidance and support.
15. Plan for Flare-Ups: If you have a chronic condition that causes epigastric pain, develop a plan for managing flare-ups. This plan may include specific medications or coping strategies to use when symptoms worsen.
Coping with epigastric pain is a multidimensional process, and it often requires a combination of medical treatments, lifestyle changes, and emotional support. Remember that it’s essential to work closely with your healthcare provider to develop a comprehensive management plan that addresses your unique needs and circumstances.

Conclusion
Epigastric pain, characterized by discomfort in the upper abdominal area, can have a profound impact on an individual’s life. The causes of epigastric pain are diverse, ranging from benign issues like indigestion and gastritis to more serious conditions such as peptic ulcers, gallstones, and even cardiac problems. The impact of epigastric pain extends beyond the physical aspect, affecting one’s emotional well-being and overall quality of life.
The key takeaway from this comprehensive guide on epigastric pain is the importance of seeking timely medical help. Whether you experience mild, intermittent discomfort or severe, persistent pain, it’s essential to consult a healthcare provider. Prompt medical evaluation can lead to an accurate diagnosis and an effective treatment plan tailored to your specific condition.
The diagnostic process often involves a combination of medical history, physical examination, and various imaging and laboratory tests. Once the underlying cause is identified, treatments may range from lifestyle modifications and medications to surgical interventions, depending on the severity and nature of the condition.
Understanding the potential complications of untreated epigastric pain underscores the urgency of seeking medical attention. Complications can include esophageal damage, bleeding ulcers, perforation, cardiac events, and more. Early diagnosis and intervention are essential to prevent these severe consequences.
Furthermore, follow-up care plays a crucial role in managing epigastric pain, especially for chronic conditions. Follow-up appointments allow healthcare providers to monitor progress, adjust treatment as needed, and prevent complications. Ensuring that patients attend follow-up appointments is vital for the long-term management of epigastric pain.
Surgery may be necessary in specific cases, such as gallstones, severe gastroesophageal reflux disease (GERD), peptic ulcers, hiatal hernias, abdominal aortic aneurysms, pancreatitis, and gastrointestinal obstructions. The decision to proceed with surgery is typically made in consultation with a healthcare provider, taking into account the patient’s overall health and the specific circumstances of their condition.
Looking ahead, the future of epigastric pain management holds promise, with advancements in personalized medicine, diagnostic tools, telemedicine, minimally invasive procedures, and the integration of artificial intelligence in healthcare.
In conclusion, recognizing the causes, symptoms, and treatment options for epigastric pain empowers individuals to take an active role in their health. Early diagnosis and timely treatment are the keys to improving the quality of life for those experiencing epigastric pain. Whether you have experienced this discomfort or are seeking information for yourself or a loved one, remember that seeking medical help is the first and most crucial step on the journey to relief and improved well-being.
Frequently Asked Questions (FAQs) –
1. What is epigastric pain?
- Epigastric pain is discomfort or pain felt in the upper abdominal area, specifically between the lower ribs and the navel. The level of discomfort can vary, and it can be triggered by a range of different underlying conditions.
2. What are the common causes of epigastric pain?
- Common causes include gastritis, gastroesophageal reflux disease (GERD), peptic ulcers, and gastritis. However, it can also be caused by less common issues like abdominal aortic aneurysms and pericarditis.
3. When should I seek medical attention for epigastric pain?
- You should seek medical help if you experience severe or persistent epigastric pain, especially if it is accompanied by symptoms such as vomiting blood, dark stools, jaundice, or breathing difficulties.
4. How is epigastric pain diagnosed?
- Diagnosis typically involves a combination of medical history, physical examination, and various imaging and laboratory tests, depending on the suspected underlying cause.
5. What are the treatment options for epigastric pain?
- Treatment options vary based on the cause of the pain and may include lifestyle modifications, medications, surgery, and stress management techniques.
6. Are there any complications associated with untreated epigastric pain?
- Yes, untreated epigastric pain can lead to complications such as esophageal damage, bleeding ulcers, perforation, and cardiac events. It’s important to seek timely medical attention to prevent these consequences.
7. What is the role of follow-up care in managing epigastric pain?
- Follow-up care is essential, especially for chronic or recurring conditions, as it allows healthcare providers to monitor your progress, adjust treatment, and prevent complications.
8. How does stress impact epigastric pain?
- Stress can exacerbate epigastric pain, especially when it is a contributing factor. Stress management techniques like meditation and yoga can help alleviate symptoms.
9. Is surgery ever necessary to treat epigastric pain?
- In some cases, surgery may be necessary, depending on the underlying cause and the patient’s overall health. Surgical intervention can be required for conditions like gallstones, severe GERD, peptic ulcers, hiatal hernias, and more.
10. What does the future of epigastric pain management look like?
- The future of epigastric pain management holds promise with advancements in personalized medicine, diagnostic tools, telemedicine, minimally invasive procedures, and the integration of artificial intelligence in healthcare.
These FAQs provide a concise overview of essential information regarding epigastric pain and its management. If you have more specific questions or concerns, it’s advisable to consult with a healthcare provider for personalized guidance.

